Introduction:
Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory ailment that significantly impacts the quality of life for millions worldwide. As one of the leading causes of morbidity and mortality, COPD manifests through persistent breathing difficulties, chronic cough, and frequent exacerbations, posing serious challenges for patients and healthcare systems alike. Effective management of this condition is crucial, and at the heart of such management is the appropriate medication use. Medications play a vital role in alleviating symptoms, enhancing lung function, and reducing the frequency and severity of flare-ups. By understanding the various classes of drugs available—ranging from bronchodilators to corticosteroids—patients can work closely with their healthcare providers to create tailored treatment plans. Ultimately, the judicious use of medication not only helps to manage the debilitating effects of COPD but also empowers individuals to lead more active and fulfilling lives.
Bronchodilators: Understanding Chronic Obstructive Pulmonary Disease (COPD) and Their Mechanisms of Action
Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory condition characterized by airflow limitation and is primarily caused by long-term exposure to harmful particles or gases, most commonly from cigarette smoke. It encompasses a group of lung diseases, including emphysema and chronic bronchitis. Understanding the different types of COPD and how bronchodilators work to alleviate symptoms is crucial for effectively managing the disease.
Types of COPD
- Chronic Bronchitis: Chronic bronchitis is characterized by inflammation of the bronchial tubes (the air passages between the nose and lungs) and is defined clinically by a cough that produces mucus for at least three months in two consecutive years.
- Mechanism of Action: The inflammation causes mucus hypersecretion, which obstructs airflow. The primary pathophysiological mechanisms involved include increased mucus production, airway narrowing, and damage to the airway walls. Persistent irritation leads to structural changes, including thickening of the bronchial walls and loss of airway elasticity.
- Emphysema: Emphysema involves damage to the alveoli (air sacs) in the lungs, resulting in reduced surface area for gas exchange. It is characterized by the destruction of elastic fibers, leading to a loss of lung structure and function.
- Mechanism of Action: The loss of elastic recoil due to the destruction of alveolar walls makes it difficult to exhale air from the lungs, leading to air trapping and difficulty breathing. Reduced surface area means that less oxygen is absorbed into the bloodstream, causing hypoxemia.
- Asthmatic COPD: This subtype involves features of both asthma and COPD. Patients may experience reversible airflow obstruction typical of asthma, along with the progressive symptoms associated with COPD.
- Mechanism of Action: The inflammation in asthmatic COPD is caused by an overactive immune response. This leads to bronchoconstriction (tightening of the muscles surrounding the airways), increased mucus production, and airway inflammation. These changes can lead to intermittent and persistent airflow obstruction.
- COPD Overlap Syndrome: This condition occurs when a patient exhibits features of both COPD and other respiratory diseases, such as asthma or bronchiectasis.
- Mechanism of Action: The pathways for obstruction and inflammation may be compounded, leading to varied mechanisms of disease progression. Treatment may need to address the unique aspects of both conditions, such as eosinophilic inflammation in asthma.
Bronchodilators in COPD Management– Bronchodilators are a cornerstone in the management of COPD. They work by relaxing the muscles around the airways, increasing airflow and improving symptoms. There are several classes of bronchodilators based on their mechanism of action:
- Beta-2 Adrenergic Agonists (SABAs and LABAs)
- Short-acting beta-2 Agonists (SABAs): Such as albuterol, provide quick relief of bronchospasms and are used as rescue medications.
- Long-acting beta-2 Agonists (LABAs): Such as salmeterol and formoterol, have a longer duration of action and are used for maintenance therapy.
- Mechanism: Both SABAs and LABAs work by stimulating beta-adrenergic receptors in the smooth muscle of the airways, leading to bronchodilation and relief of symptoms.
- Anticholinergics (Muscarinic Antagonists)
- Short-acting muscarinic Antagonists (SAMAs): Such as ipratropium bromide, and long-acting muscarinic antagonists (LAMAs) like tiotropium.
- Mechanism: These medications block the action of acetylcholine at muscarinic receptors in the bronchial smooth muscle, leading to relaxation of the airways and reduced mucus secretion.
- Combination Therapy
- Patients with more severe COPD may benefit from combination therapy, which typically combines LABAs with LAMAs or inhaled corticosteroids to manage inflammation and improve lung function.
- Mechanism: Combining these agents addresses different pathways of the disease—bronchodilation from the beta-agonists and reduced inflammation from corticosteroids.
COPD is a multifaceted disease that presents significant challenges in terms of management. Understanding the types of COPD, including chronic bronchitis, emphysema, and asthmatic COPD, is crucial for tailoring treatment strategies. Bronchodilators play a pivotal role in managing symptoms and improving the quality of life for individuals with COPD. By facilitating easier breathing through various mechanisms of action, they are essential to effective COPD management and can significantly reduce the burden of this chronic disease. Regular follow-up and a comprehensive approach to treatment can help patients lead more active and fulfilling lives.
Inhaled Corticosteroids for COPD: Benefits and Potential Side Effects
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition characterized by airflow limitation which can severely impact an individual’s quality of life. Among various treatment modalities available, inhaled corticosteroids (ICS) have emerged as a cornerstone in managing COPD, particularly in patients with frequent exacerbations. This article delves into the benefits of inhaled corticosteroids for COPD management, as well as their potential side effects.
Benefits of Inhaled Corticosteroids
- Reduction of Inflammation: COPD exacerbations are often driven by inflammation in the airways. Inhaled corticosteroids target this inflammation directly, providing symptomatic relief and improving lung function. By reducing the inflammatory response, patients often experience less wheezing, coughing, and shortness of breath.
- Decreased Frequency of Exacerbations: One of the most significant advantages of using inhaled corticosteroids in COPD is their ability to reduce the frequency of exacerbations. These exacerbations can be debilitating and lead to hospitalizations. Research indicates that ICS can lower the incidence of these events, which can result in improved overall stability for patients.
- Improved Quality of Life: The alleviation of symptoms and reduction in exacerbations contribute to an enhanced quality of life for individuals suffering from COPD. Patients using ICS may find it easier to engage in daily activities, leading to better physical and emotional well-being.
- Potential Survival Benefit: Some studies have suggested that long-term use of inhaled corticosteroids may be associated with a reduction in mortality among COPD patients. However, this remains a point of ongoing research and debate, and more conclusive evidence is needed.
- Synergistic Effects: ICS are often used in conjunction with long-acting bronchodilators (LABAs) to maximize therapeutic effects. This combination therapy helps to open the airways and reduce inflammation simultaneously, leading to improved lung function and symptom control.
Potential Side Effects
While inhaled corticosteroids are beneficial in managing COPD, they are not without their potential side effects:
- Oral Candidiasis: One of the most common side effects associated with ICS use is oral thrush or oropharyngeal candidiasis. The inhalation of corticosteroids can alter the oral microbiome, leading to fungal overgrowth. Patients are often advised to rinse their mouths after inhalation to mitigate this risk.
- Dysphonia: Patients may experience hoarseness or changes in their voice due to the local effects of corticosteroids on the larynx and vocal cords. This can be distressing for some individuals, particularly those who rely on their voice for work.
- Systemic Effects: Although the systemic absorption of inhaled corticosteroids is much lower than that of oral corticosteroids, prolonged use can still lead to systemic side effects, such as weight gain, osteoporosis, hypertension, and diabetes. However, these risks are generally lower with inhaled forms compared to systemic corticosteroids.
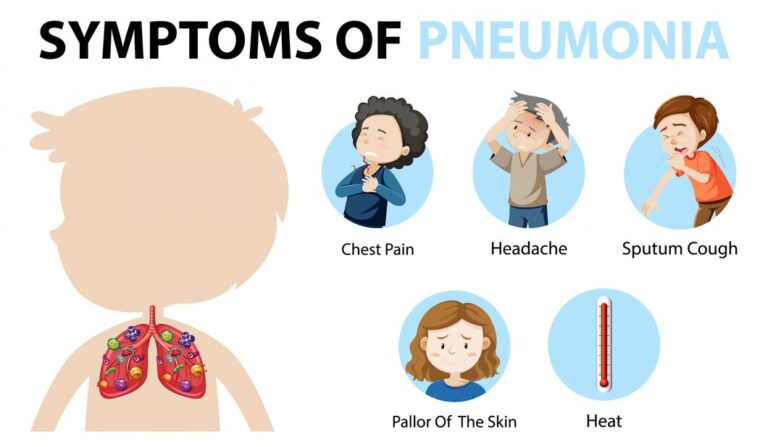
- Pneumonia Risk: Some studies indicate an increased risk of pneumonia among COPD patients using inhaled corticosteroids, particularly at higher doses. This is thought to be related to the effects of corticosteroids on the immune response in the lungs.
- Adrenal Suppression: Long-term use of inhaled corticosteroids can, though rarely, lead to adrenal suppression. This can result in the body’s impaired ability to respond to stress, leading to complications, especially during illness or surgery.
Inhaled corticosteroids play a vital role in the management of COPD, particularly for patients with persistent symptoms and frequent exacerbations. They offer a range of benefits, including reduced airway inflammation, a decrease in the frequency of exacerbations, and improved quality of life. However, healthcare providers must carefully weigh these benefits against potential side effects and monitor patients closely to minimize risks. Ultimately, the decision to use ICS should involve a personalized approach tailored to the individual needs and health status of each COPD patient, incorporating regular assessments and adjustments as necessary.
Other Medications for COPD: A Comprehensive Overview
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by obstructed airflow that interferes with normal breathing. While bronchodilators and corticosteroids are commonly recognized as the cornerstone pharmacological treatments for managing COPD symptoms, other therapeutic options play a crucial role in optimizing patient care. This article explores alternative treatments, including antibiotics, oxygen therapy, and pulmonary rehabilitation, which can significantly enhance the quality of life for individuals living with COPD.
- Antibiotics: Managing Exacerbations
- Patients with COPD frequently experience exacerbations, which are sudden flare-ups of symptoms such as increased breathlessness, coughing, and sputum production. These exacerbations are often triggered by respiratory infections, predominantly bacterial. In these situations, antibiotics are prescribed to curtail the infection and alleviate symptoms. Commonly used antibiotics for COPD exacerbations include:
- Amoxicillin and Doxycycline: Effective against common pathogens like Haemophilus influenzae and Streptococcus pneumoniae.
- Macrolides: Drugs such as Azithromycin can help address atypical infections and possess additional anti-inflammatory properties.
- Patients need to receive appropriate antibiotic therapy, as misuse or overuse can lead to antibiotic resistance. Therefore, clinicians typically evaluate the severity of the exacerbation and the presence of bacterial infection before initiating antibiotics.
- Patients with COPD frequently experience exacerbations, which are sudden flare-ups of symptoms such as increased breathlessness, coughing, and sputum production. These exacerbations are often triggered by respiratory infections, predominantly bacterial. In these situations, antibiotics are prescribed to curtail the infection and alleviate symptoms. Commonly used antibiotics for COPD exacerbations include:
- Oxygen Therapy: Enhancing Oxygenation
- For many COPD patients, especially those with severe disease or significant hypoxemia (low blood oxygen levels), supplemental oxygen therapy becomes a critical element of treatment. Oxygen therapy works by delivering additional oxygen to the lungs and improving overall oxygen saturation in the bloodstream.
- Patients may require long-term oxygen therapy (LTOT) if their oxygen levels are consistently below 88% during rest or sleep. Benefits of oxygen therapy include:
- Improved exercise capacity: Enhanced oxygenation helps patients engage in physical activities with greater ease.
- Reduced strain on the heart: Sufficient oxygen levels can alleviate right heart strain, lowering the risk of cor pulmonale (right-sided heart failure due to lung disease).
- Better sleep quality: Oxygen therapy can reduce symptoms of nocturnal hypoxemia, leading to improved sleep patterns.
- Patients should undergo thorough evaluations to determine the need for oxygen therapy, and healthcare providers must guide its proper use to ensure safety and effectiveness.
- Pulmonary Rehabilitation: A Holistic Approach
- Pulmonary rehabilitation is an essential component of comprehensive COPD management. This multidisciplinary program encompasses exercise training, health education, and psychosocial support tailored to meet the specific needs of COPD patients. The goals of pulmonary rehabilitation are to improve overall physical fitness, enhance quality of life, and empower patients to manage their condition effectively.
- Key components of pulmonary rehabilitation include:
- Exercise Training: Tailored exercise regimens improve muscle strength and endurance. Walking, cycling, and aerobic activities help patients boost cardiovascular health and reduce breathlessness.
- Education and Self-Management: Patients learn about their disease, medications, and self-monitoring techniques. Understanding triggers and symptoms enables patients to proactively manage exacerbations, thus improving their independence.
- Nutritional Support: Proper nutrition is emphasized since many COPD patients experience weight loss and malnutrition. Dietitians often contribute to ensuring patients receive adequate caloric intake and essential nutrients to support their overall health.
- Psychosocial Support: Emotional well-being is crucial in managing a chronic disease. Counseling and support groups can aid patients in coping with anxiety, depression, and other psychological aspects of living with COPD.
- While the primary medications for COPD often dominate discussions around treatment, other therapies such as antibiotics, oxygen therapy, and pulmonary rehabilitation are equally important in comprehensive disease management. By incorporating these interventions into a holistic care plan, healthcare providers can significantly improve health outcomes and enhance the quality of life for individuals living with COPD. Patients are encouraged to work closely with their healthcare team to devise a personalized management plan that addresses their unique needs, enabling them to live their lives to the fullest despite the challenges of this chronic condition.
Importance of Compliance in COPD: The Role of Patient Adherence to Medication Regimens
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition encompassing chronic bronchitis and emphysema, characterized by airflow limitation and difficulty breathing. Its management requires a multifaceted approach, and one of the most critical components is patient adherence to prescribed medication regimens. Compliance with treatment not only improves patients’ quality of life but also significantly impacts the trajectory of the disease. This article delves into the importance of compliance in COPD management and the vital role of patient adherence to medication.
- Understanding COPD and its Challenges
- COPD remains a leading cause of morbidity and mortality worldwide, affecting millions of people. The disease is primarily caused by long-term exposure to harmful substances, such as tobacco smoke, air pollution, and occupational dust, resulting in chronic inflammation and damage to the airways and lung tissue. Symptoms include persistent cough, sputum production, and shortness of breath, significantly impairing daily activities.
- Despite the availability of various pharmacological interventions—such as bronchodilators, corticosteroids, and pulmonary rehabilitation—the effectiveness of these treatments hinges on patients’ adherence to their prescribed medication regimens. Non-compliance is rampant, with studies suggesting that a significant percentage of COPD patients do not take their medications as directed, leading to worsening symptoms, increased hospitalizations, and declining overall health.
- The Link Between Medication Adherence and Health Outcomes
- Adherence to medication regimens is paramount for several reasons:
- Symptom Control and Improved Quality of Life
- Regular use of prescribed medications is essential for controlling the symptoms of COPD. Bronchodilators help alleviate breathlessness and improve exercise capacity, while inhaled corticosteroids reduce inflammation and frequency of exacerbations. Adherence to these medications can lead to better symptom management, allowing patients to maintain an active and fulfilling lifestyle.
- Reduced Exacerbation Rates
- Non-adherence to maintenance therapy often results in increased exacerbation rates. These episodes of acute worsening of symptoms not only lead to distress and reduced quality of life but can also result in hospitalization and increased healthcare costs. By adhering to a consistent medication regimen, patients can significantly decrease the frequency and severity of exacerbations, contributing to long-term disease stability.
- Prevention of Disease Progression
- While COPD is a progressive disease, medication adherence can slow its progression. Regular use of maintenance medications can help preserve lung function and improve overall health outcomes. Conversely, non-compliance may accelerate deterioration, leading to a cycle of worsening symptoms and further non-adherence due to increased anxiety and fear of physical limitations.
- Cost-Effectiveness
- Adherence to medication not only benefits patients’ health but also has significant economic implications. Reducing exacerbation rates and hospitalizations leads to lower healthcare costs over time. By prioritizing adherence, patients play a vital role in mitigating the financial burden of COPD—both on themselves and the healthcare system.
- Symptom Control and Improved Quality of Life
- Adherence to medication regimens is paramount for several reasons:
- Barriers to Compliance and Strategies for Improvement
- Understanding the barriers to adherence is crucial for effective intervention. Common challenges include:
- Complexity of Medication Regimens: Multiple medications, often prescribed in different dosages at varying times, can overwhelm patients.
- Side Effects: Concerns about potential side effects may lead patients to skip doses or discontinue medications.
- Lack of Understanding: Patients may not fully comprehend the importance of their medications or how to properly use inhalers.
- Psychological Factors: Depression and anxiety, prevalent in COPD patients, can negatively influence motivation and adherence.
- Understanding the barriers to adherence is crucial for effective intervention. Common challenges include:
- Strategies to Enhance Adherence
- To improve medication adherence, healthcare professionals can employ several strategies:
- Education and Counseling: Providing clear, concise information regarding the role of medications in managing COPD can empower patients. Teaching proper inhaler techniques and the importance of each medication fosters understanding and commitment.
- Simplification of Regimens: Whenever possible, clinicians should aim to prescribe fewer medications or combination therapies, simplifying the patient’s treatment plan to enhance adherence.
- Regular Follow-Up: Establishing a system of regular follow-ups allows healthcare providers to assess adherence, address barriers, and modify treatment plans as necessary.
- Use of Technology: Consideration of mobile apps or reminders can assist patients in keeping track of their medication schedules, promoting adherence.
- Supporting Psychological Well-being: Addressing mental health concerns and providing support through counseling or support groups can enhance patients’ motivation to adhere to treatment.
- Adherence to medication regimens is a critical facet of managing Chronic Obstructive Pulmonary Disease. It plays a pivotal role in controlling symptoms, reducing exacerbation rates, preventing disease progression, and minimizing healthcare costs. As healthcare providers, it is our responsibility to support patients in their journey toward adherence, addressing barriers and employing strategies to facilitate better health outcomes. Ultimately, improved patient adherence empowers individuals to take charge of their health, fostering independence and a better quality of life amidst the challenges of COPD. Through collaboration between patients and healthcare professionals, we can transform COPD management and enhance the lives of those affected by this debilitating disease.
- To improve medication adherence, healthcare professionals can employ several strategies:
Conclusion
Medications play a pivotal role in the management of Chronic Obstructive Pulmonary Disease (COPD). They help to alleviate symptoms, improve quality of life, reduce the frequency and severity of exacerbations, and slow the progression of the disease. Bronchodilators, corticosteroids, phosphodiesterase-4 inhibitors, and antibiotics are commonly used to manage COPD symptoms and complications. While medications are not a cure for COPD, they are essential in providing relief and maintaining lung function. Patients must adhere to their prescribed medication regimens and work closely with their healthcare providers to optimize treatment plans and adjust medications as needed. Effective COPD management often involves a comprehensive approach, combining medication with lifestyle modifications, pulmonary rehabilitation, and regular medical follow-ups to achieve the best possible outcomes.